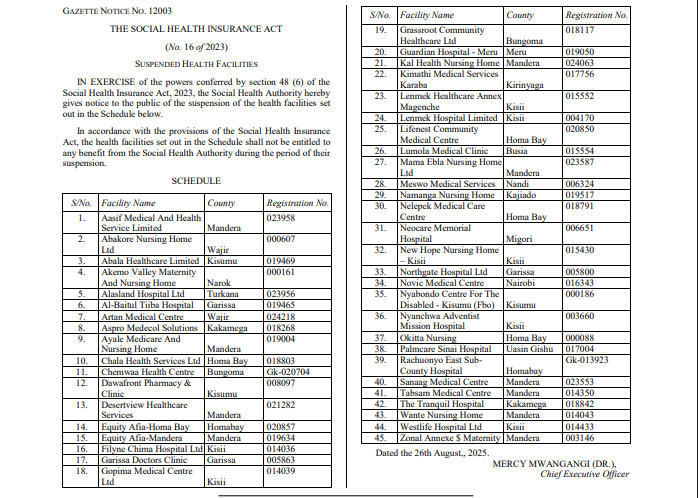
Following comprehensive investigations, the Social Health Authority (SHA) has suspended 45 health facilities from providing services under the Social Health Insurance program.
In a gazette notice published on Tuesday, August 26, the authority noted that the suspended facilities are barred from offering services to SHA beneficiaries during their suspension.
"In accordance with the provisions of the Social Health Insurance Act, the facilities listed in the Schedule shall not be entitled to any benefit from the Social Health Authority during their suspension,” the gazette notice reads.
The suspensions came after Health Cabinet Secretary Aden Duale revealed disturbing fraud patterns among healthcare facilities, including bill inflation, falsified records, and claims for services never provided to patients.
The suspended facilities span multiple counties, affecting healthcare access in various regions.
Read More
The highest number was in Mandera County, where eight facilities, including Aaref Medical and Health Service Limited, Ayale Medicare and Nursing Home, Desertview Healthcare Services, Mama Elba Nursing Home Limited, Sanaag Medical Centre, Tabsam Medical Centre, Wante Nursing Home, and Zonal Annex and Maternity, have been suspended.
Kisii County has also seen significant enforcement action with multiple facilities affected, including Filyne Chima Hospital Limited, Gopima Medical Centre, Lemmek Healthcare Annex Magenche, Lemmek Hospital Limited, New Hope Nursing Home-Kisii, Nyanchwa Adventist Mission Hospital, and Westlife Hospital Limited.
Other affected counties include Kisumu, Turkana, Kakamega, Homa Bay, Meru, Migori, and Kirinyaga counties.
The suspensions represent the latest development in SHA's crackdown on fraudulent practices within the health insurance system.
Earlier investigations by the Ministry of Health revealed systematic attempts to defraud the public health insurance scheme through various methods.
On Monday, Health CS Duale disclosed that audit findings showed healthcare facilities engaging in "upcoding" practices, where patients were charged for more expensive procedures than those performed. This practice allowed facilities to claim higher reimbursements from the insurance scheme while providing lower-cost services.
The investigations also uncovered systematic falsification of medical records, with some facilities creating or altering documentation to support fraudulent claims. This violated both the Social Health Insurance Act and its accompanying regulations, undermining the integrity of the healthcare financing system.
Particularly concerning was the discovery of facilities illegally converting outpatient visits to inpatient admissions, enabling them to claim significantly higher reimbursement rates.






